The Hidden Link Between Trauma and Addiction
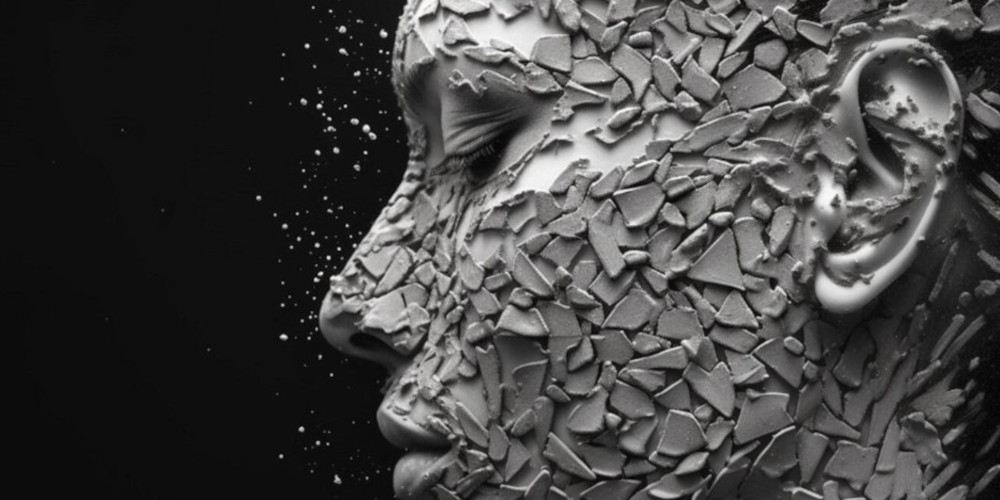
The Wounds You Can’t See Shape the Behaviours You Do
Trauma is not always dramatic or obvious. It is not limited to violence, accidents, disasters, or extreme events. Trauma often hides inside moments that felt too overwhelming for a person to process at the time. It settles into the nervous system quietly, shaping how someone responds to stress, relationships, conflict, and emotional discomfort. When trauma goes unrecognised or unspoken, it becomes a silent architect of behaviour. It influences everything from how a person copes to how they connect, withdraw, react, or shut down. Addiction finds fertile ground in those invisible injuries because unresolved trauma creates emotional pain that demands relief, and substances offer that relief with terrifying efficiency.
People rarely set out to become dependent on alcohol, drugs, gambling, or any compulsive behaviour. They look for escape from emotional noise they do not have the tools to manage. Trauma creates that noise. It distorts a person’s emotional baseline, making everyday stress feel heavier than it should. Trauma makes the nervous system reactive, the mind unsettled, and the body tense. Substances become a shortcut to temporary calm, which the traumatised system interprets as safety. Eventually, the substance becomes part of how the person survives the discomfort trauma left behind. This is why the link between trauma and addiction is so strong: both are rooted in self-protection, even when the consequences are harmful.
Why the Brain Turns to Substances After Trauma
The human brain is wired for survival. When someone experiences trauma, the brain rewires itself in ways that prioritise avoidance of further pain. It heightens vigilance, narrows emotional tolerance, and increases sensitivity to stress. For many people, especially those who never learned emotional regulation skills, trauma creates inner chaos that feels impossible to manage. Substances step in as a kind of emotional anaesthetic. They quiet intrusive thoughts. They soften intense emotions. They reduce anxiety temporarily. They make sleep possible. They create a few hours of distance from memories or fears that feel too heavy to carry.
The brain quickly learns to associate the substance with safety. This association has nothing to do with weakness or flawed character. It is a neurological adaptation. Once that link forms, cravings become conditioned responses to emotional triggers rather than conscious desires. The person is not chasing pleasure; they are chasing relief from an internal state that feels unbearable. This is why telling someone to “just stop” misses the entire reality of trauma-driven addiction. Without healing the underlying emotional injury, asking someone to stop using the only tool they believe works feels impossible and unsafe.
How Trauma Shapes the Emotional Landscape That Fuels Addiction
Trauma alters a person’s ability to regulate emotions long before addiction develops. Someone who experienced trauma may struggle with sudden waves of anxiety, emotional numbness, irritability, shame, anger, or a sense of emptiness they cannot explain. Ordinary challenges feel overwhelming because trauma distorts how the mind interprets stress. Emotional triggers become unpredictable. Relationships feel complicated. Trust becomes fragile. Vulnerability feels dangerous.
Addiction often begins when the person discovers that a substance or behaviour temporarily stabilises this emotional chaos. Alcohol may soften anxiety. Drugs may quiet intrusive memories. Gambling may provide distraction and reward. Prescription medication may provide artificial calm. The relief is real but short-lived, and the cost is enormous. Over time, the brain becomes dependent not because it craves the substance, but because it craves the emotional stability it believes the substance provides.
The Cycle of Trauma and Addiction Reinforces Itself
Once someone begins using substances to cope with trauma, the addiction itself creates new sources of shame, secrecy, relationship strain, and self-blame. These new emotional injuries feed back into the original trauma, intensifying it. The person then uses more to numb the worsening emotional pain, which in turn creates further consequences. This cycle traps people not because they lack discipline but because they are trying to survive a storm of unprocessed emotion with tools that were never meant to carry such a burden.
Families often misinterpret this cycle as selfishness, irresponsibility, or stubbornness. In reality, the person is caught between wanting relief and fearing the consequences of seeking it. Trauma complicates every choice. The addicted behaviour becomes both the problem and the attempted solution. This is why trauma and addiction must be treated together. Focusing on the substance without addressing the trauma leaves the person exposed to the same emotional triggers that drove the addiction in the first place.
Misunderstand the Trauma-Addiction Connection
Trauma is not always recognised because many people believe trauma requires extreme events. They assume trauma needs to be dramatic or obvious. But trauma can come from growing up in a home where emotional needs were neglected, where voices were loud and unpredictable, where affection was inconsistent, or where pressure to perform overshadowed emotional safety. Trauma can come from bullying, abandonment, betrayal, humiliation, or chronic stress. It can come from loss that was never processed. Trauma does not need to be cinematic to be deeply damaging.
People often minimise their own trauma because it doesn’t fit the stereotype. They believe others had it worse, so their pain must not count. This belief prevents many people from recognising why they use substances in the first place. When you believe your trauma “doesn’t count,” you also believe you should be coping better, which fuels shame. Shame is one of addiction’s strongest accelerators. Understanding trauma allows people to see their behaviour not as failure, but as a response to pain they were never taught to manage.
Why Treating Only the Addiction Doesn’t Work
Rehab programmes that focus solely on detox and abstinence often fail because they treat the addiction in isolation. If the underlying trauma remains untouched, the emotional triggers remain alive. The person leaves treatment with their substance removed but their pain intact. Without new coping mechanisms, the nervous system returns to its old strategies when stress or emotional overwhelm strikes. Detox clears the body, but trauma remains in the mind and the nervous system. This is why relapse often happens when life becomes challenging again. The person is not choosing relapse; they are responding to unaddressed trauma that has resurfaced.
Treatment must address both sides: the behaviour and the emotional injury beneath it. Trauma-informed therapy, specialised counselling, structured emotional regulation strategies, and professional guidance help people understand the roots of their addiction. They learn how to respond to their internal world without leaning on substances. They learn the skills they never received earlier in life. This is not about dwelling on the past; it is about freeing the present from what the past left behind.
Why Trauma-Informed Treatment Changes Everything
Trauma-informed treatment acknowledges that the person’s behaviour is connected to emotional pain rather than moral failure. It shifts the focus from stopping the substance to understanding the emotional injuries the substance was soothing. Professionals trained in trauma recognise the signs that others miss. They understand how trauma affects the nervous system, how it shapes self-perception, and how it influences relationships. They guide people in stabilising their internal world so that they no longer need substances to cope.
This form of treatment teaches people how to interpret their emotional triggers, how to manage overwhelming feelings, how to build healthy boundaries, and how to regulate their nervous system. Recovery becomes grounded in emotional safety rather than fear, shame, or control. When trauma is addressed directly, the addiction loses the psychological foundation that kept it alive.
Breaking the Cycle
Families often want to help but do not know how. Their approach may be shaped by frustration, confusion, or fear. Without understanding trauma, families misinterpret behaviour. They pressure the person to simply stop. They focus on the addiction rather than the emotional injury underneath. This often leads to conflict because it addresses symptoms rather than causes. Families who understand the trauma-addiction connection are better able to support real change. They recognise that healing requires emotional safety, not shame. They learn that boundaries are essential but must be delivered without hostility. They understand that recovery is not about forcing willpower but building new emotional tools.
Families also need support because trauma does not only affect the person with the addiction. It affects the entire household. People absorb tension, anxiety, and emotional wear. Families often carry secondary trauma from repeated crises and disappointments. They need guidance just as much as the person struggling, and trauma-informed family counselling can restore stability that addiction eroded.
Healing Trauma Is Not About Rewriting History
Healing trauma does not require reliving every painful detail. It requires understanding how the past shaped emotional responses, beliefs, and patterns. It requires building new neural pathways that respond to stress differently. It requires learning how to feel without drowning, how to calm the nervous system without substances, and how to relate to others without fear or withdrawal.
When trauma is addressed, people no longer feel controlled by emotional chaos. The addiction loses its role as a coping mechanism. Recovery becomes grounded, not fragile. It becomes something built on understanding rather than willpower, on emotional clarity rather than fear, and on genuine support rather than isolation.
The Path to Recovery
Addiction is rarely about the substance alone. It is about the pain underneath, the memories never processed, the emotions never expressed, and the experiences never fully understood. Trauma shapes the emotional landscape long before addiction enters the picture. Treating one without acknowledging the other leaves the cycle intact.
The moment trauma is recognised, the entire narrative shifts. The person sees themselves with compassion rather than shame. The family sees the behaviour through a lens of understanding rather than anger. Treatment becomes effective because it addresses the root, not just the symptom.
Healing begins when people finally stop fighting the surface and start understanding the depth. Trauma may have shaped the past, but it does not need to shape the future. When trauma and addiction are treated together, recovery becomes not just possible but sustainable, anchored in emotional truth rather than temporary escape.

